
General Information
Arthritis is the leading cause of disability in the U.S. In 1998, arthritis and other rheumatic conditions affected 43 million people – a number that is expected to climb to 60 million by 2020 as the “baby boom” generation ages. That’s almost 20 percent of the population.

Arthritis conditions don’t usually cause death, but they do worsen health-related quality of life. Arthritis is the leading cause of disability in the United States, limiting the everyday activities of more than 7 million Americans. Arthritis results in 39 million physician visits and almost 2.5 million hospitalizations each year.
Findings on the impact of arthritis by the Centers for Disease Control and Prevention (CDC) show people with arthritis have worse health-related quality of life than people without it, regardless of sex, age or education level. From 1996-98, the CDC interviewed more than 32,000 people in 11 states about:
- Their general self-rated health.
- The frequency of days in which their physical health was not good.
- The frequency of days in which their mental health was not good.
- The frequency of days in which their usual activities were limited.
Overall, the CDC found about 29 percent of people with arthritis. Doctors had diagnosed most of these people (75 percent). Others had symptoms of pain, aching, stiffness or swelling in or around a joint on most days for at least a month.
People with arthritis reported having fair or poor health about three times more often than did people without arthritis. The CDC says “unhealthy days” are days in which physical and/or mental health was not good. Among arthritis sufferers, the most unhealthy days were experienced by women, younger people, and people with less than a college education. For people with less education, unhealthy days may reflect less access to health care or more physical labor, the CDC says. Depression is common in people with all types of arthritis, especially rheumatoid.
Prevailing myths have portrayed arthritis as an inevitable part of aging that can only be endured. But the CDC says there are effective interventions that are available to prevent or reduce arthritis-related pain and disability. These include early diagnosis and appropriate management, including weight control, physical activity, physical and occupational therapy and joint replacement, when necessary.
Joints & Cartilage
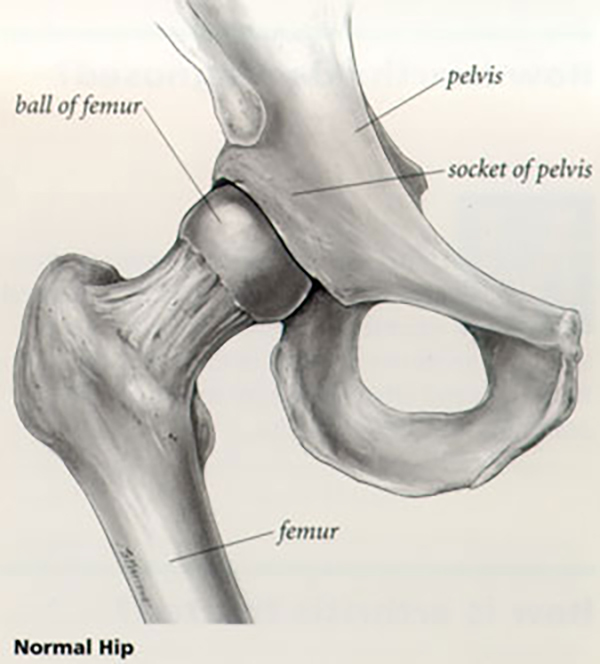
A joint is where the ends of two or more bones meet. For example, a bone of the lower leg, called the shin or tibia and the thighbone, called the femur, meet to form the knee joint. The hip is a ball and socket joint. It is formed by the upper end of the thighbone-the ball-fitting into the socket-part of the pelvis called the acetabulum.
The bone ends of a joint are covered with a smooth material called cartilage. The cartilage cushions the bone and allows the joint to move easily without pain. The joint is enclosed by a fibrous envelope called the synovium which produces a fluid that helps to reduce friction and wear in a joint. Ligaments connect the bones and keep the joint stable. Muscles and tendons power the joint and enable it to move.
Inflammation
Inflammation is one of the body’s normal reactions to injury or disease. In an injured or diseased joint, this results in swelling, pain, and stiffness. Inflammation is usually temporary, but in arthritic joints, it may cause long-lasting or permanent disability.
Types of Arthritis
There are more than 100 different types of arthritis. This web site has pages which describe in symptoms, care and treatment of the following:
Osteoarthritis
The most common type of arthritis is osteoarthritis. It is seen in many people as they age, although it may begin when they are younger as a result of injury or overuse. All joints may be more affected if they are used extensively in work or sports, or if they have been damaged from fractures or other injuries. Read more about osteoarthritis.
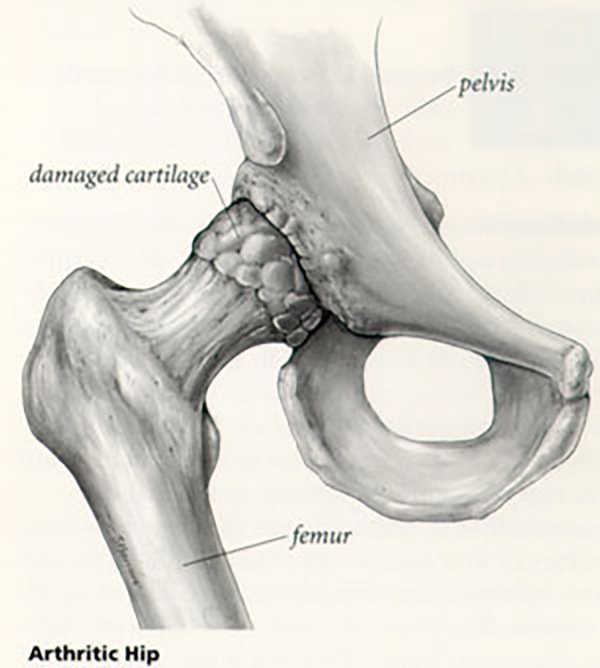
In osteoarthritis, the cartilage covering the bone ends gradually wears away. In many cases, bone growths called “spurs” can develop in osteoarthritic joints. The joint inflammation causes pain and swelling. Continued use of the joint produces pain. Some relief may be possible through rest or modified activity.
Rheumatoid arthritis
Rheumatoid arthritis is a long-lasting disease that can affect many parts of the body, including the joints. In rheumatoid arthritis, the joint lining swells, invading surrounding tissues, and producing chemical substances that attack and destroy the joint surface. This commonly occurs in joints in the hands and feet. Larger joints such as hips, knees, and elbows also may be involved. Swelling, pain, and stiffness are usually present even when the joint is not used. Rheumatoid arthritis can affect people of all ages, even children. However, more than 70 percent of people with this disease are over 30 years old. Many joints of the body may be involved at the same time.
Treatment Options for Arthritis
Medications
Many over-the-counter medications, including aspirin, ibuprofen, and naproxen (common anti-inflammatory drugs) may be used to effectively control pain and inflammation in arthritis. Acetaminophen (Tylenol) may be used to effectively control pain. Prescription medications also are available if over-the-counter medications are not effective. The physician chooses a medication by taking into account the type of arthritis, its severity, and the patient’s general physical health. Patients with ulcers, asthma, kidney, or liver disease may not be able to safely take anti-inflammatory medications. Injections of liquid cortisone directly into the joint may temporarily help to relieve pain and swelling. It is important to know, however, that repeated frequent injections into the same joint can damage the joint and have undesirable side effects.
Joint Protection
Canes, crutches, walkers, or splints may help relieve the stress and strain on arthritic joints. Learning methods of performing daily activities that are the less stressful to painful joints also may be helpful. Certain exercises and physical therapy (such as heat treatments) may be used to decrease stiffness and to strengthen the weakened muscles around the joint.
Surgery
In general, surgery for arthritis can be effective at pain relief when other methods of nonsurgical treatment have failed. The physician and patient will choose the type of surgery by taking into account the type of arthritis, its severity, and the patient’s physical condition. Surgical procedures include:
- removal of the diseased or damaged joint lining;
- realignment of the joints;
- total joint replacement; and
- fusion of the bone ends of a joint to prevent joint motion and relieve joint pain.
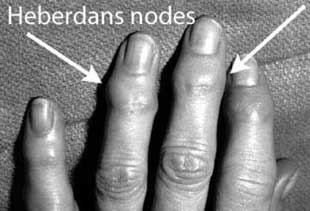 Heberden nodes are “bumps” which occur at the last joint of the finger or thumb due to wear and tear arthritis (osteoarthritis). As the joints deteriorate, small bone spurs form over the back of the joints and make them appear “lumpy.” Since most Heberden nodes are not painful and seldom interfere with function, no specific treatment is usually required. Patients with pain can be treated with anti-inflammatory medications. All patients should continue moving their hands; disuse frequently results in stiffness.
Heberden nodes are “bumps” which occur at the last joint of the finger or thumb due to wear and tear arthritis (osteoarthritis). As the joints deteriorate, small bone spurs form over the back of the joints and make them appear “lumpy.” Since most Heberden nodes are not painful and seldom interfere with function, no specific treatment is usually required. Patients with pain can be treated with anti-inflammatory medications. All patients should continue moving their hands; disuse frequently results in stiffness.
Is Their a Cure for Arthritis?
 At present, most types of arthritis cannot be cured. Researchers continue to make progress in finding the underlying causes for the major types of arthritis. In most cases, persons with arthritis can continue to perform normal activities of daily living. Exercise programs, anti-inflammatory drugs, and weight reduction for obese persons are common measures to reduce pain, stiffness, and improve function.
At present, most types of arthritis cannot be cured. Researchers continue to make progress in finding the underlying causes for the major types of arthritis. In most cases, persons with arthritis can continue to perform normal activities of daily living. Exercise programs, anti-inflammatory drugs, and weight reduction for obese persons are common measures to reduce pain, stiffness, and improve function.
In persons with severe cases of arthritis, surgery can often provide dramatic pain relief and restore lost joint function. Some types of arthritis, such as rheumatoid arthritis, are often treated by a team of health care professionals. These professionals may include rheumatologists, physical and occupational therapists, social workers, rehabilitation specialists, and hand surgeon.
Dr. Concannon is a medical doctor with extensive training in the diagnosis and nonsurgical and surgical treatment of the hand, including bones, joints, ligaments, tendons, muscles and nerves.
Arthritis can affect any joint in the body, but it is most visible when it strikes the hands and fingers. Each hand has 27 bones plus the two bones of the forearm that help define the wrist. Joints are created whenever two or more bones come together, so there is plenty of potential for arthritic problems in the hand.
Symptoms of Arthritis
Stiffness, swelling, loss of motion, and pain are symptoms common to both osteoarthritis and rheumatoid arthritis in the hand. With osteoarthritis, bony nodules may develop at the middle joints of one or more fingers (Bouchard’s nodes) and at the finger tip (Heberden’s nodes). The joints become enlarged and the fingers crooked. In rheumatoid arthritis, some joints may be more swollen than others. There is often a sausage-shaped (fusiform) swelling of the finger. Other symptoms of rheumatoid arthritis of the hand include:
- a soft, lumpy mass over the back of the hand
- a creaking sound (crepitus) during movement
- a shift in the position of the fingers as they drift away from the direction of the thumb
- inflammation of the finger tendons, resulting in a permanent bending (Boutonnière) deformity
- a “swan’s neck” deformity caused by hyperextension (sway-back) at the middle joint of the finger associated with a bent fingertip
Diagnosis
 Your doctor will examine you and ask whether you have similar symptoms in other joints. X-rays will show certain characteristics of arthritis, such as a narrowing of the joint space, the formation of cysts or bony outgrowths (osteophytes or “nodes”) and the development of hard (sclerotic) areas of bone. If your doctor suspects rheumatoid arthritis, he or she may request blood or other lab tests to confirm the diagnosis.
Your doctor will examine you and ask whether you have similar symptoms in other joints. X-rays will show certain characteristics of arthritis, such as a narrowing of the joint space, the formation of cysts or bony outgrowths (osteophytes or “nodes”) and the development of hard (sclerotic) areas of bone. If your doctor suspects rheumatoid arthritis, he or she may request blood or other lab tests to confirm the diagnosis.
Treatments
Treatment is designed to relieve pain and restore function. Treatment decisions are based on the type of arthritis you have, its progression and its impact on your life. Anti-inflammatory medications such as aspirin or ibuprofen may help reduce swelling and relieve pain; prescription medications or steroid (cortisone) injections may be recommended. Your physician may refer you to a physical or occupational therapist because changing the way you do things with your hands may help relieve pain and pressure.
Osteoarthritis treatments
If you have osteoarthritis, your physician may recommend a period of rest. You may also be advised to wear finger or wrist splints at night and for selected activities. Surgery is usually not advised unless these treatments fail. Several surgical options are available:
- Surgery may be used to drain or remove the cysts associated with the nodes and to remove excess bone growth.
- Joint fusion (stiffening the problem joint) may be used to correct deformities that interfere with functioning or that are cosmetically unacceptable.
- A joint replacement may be advised.
Rheumatoid arthritis treatments
If you have rheumatoid arthritis in your hands, medications can help decrease inflammation, relieve pain and retard the progress of the disease. Rest, controlled exercise, and wearing finger or wrist splints may also be part of your treatment program. Several disease-modifying treatments are now available. These include cortisone injections, antimalarial drugs, methotrexate, cyclosporine, gold and some other drugs that help suppress the body’s immune system to reduce the inflammation. Adaptive devices may help you cope with the activities of daily living.
Rheumatoid arthritis often affects the connective tissues (tendons) as well as the joints. The tendons that become inflamed may rupture. If this happens, you may be unable to bend or straighten your fingers or to grip properly. In certain cases, specific preventive surgery may be recommended. Preventive surgery options include removing nodules, releasing pressure on tendons by removing the inflamed tissue, and strengthening the tendons. If a tendon rupture occurs, a hand surgeon may be able to repair it with a tendon “transfer” or graft. Unfortunately, there is no cure for rheumatoid arthritis. However, surgical procedures can often help correct deformities, relieve pain, and improve function. These options include joint replacements, joint fusion and, in some cases, removing damaged bone. Examples of severe osteoarthritis of the DIP joints of the hand. The bony osteophytes that form at these joints are often painful, and contribute to the external deformity as well.
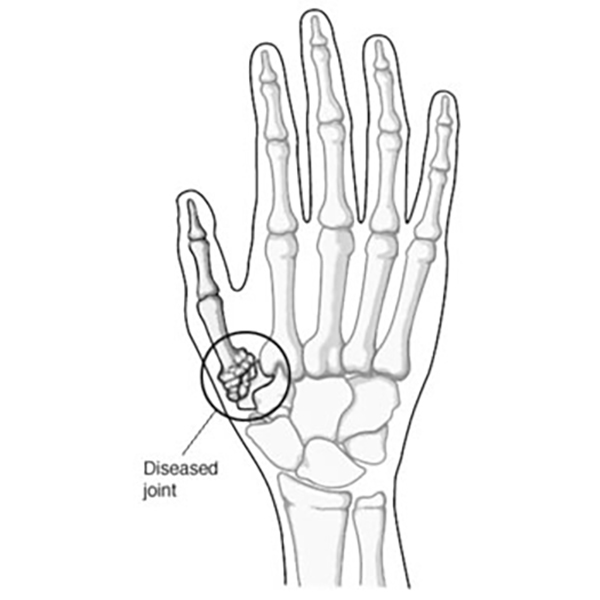
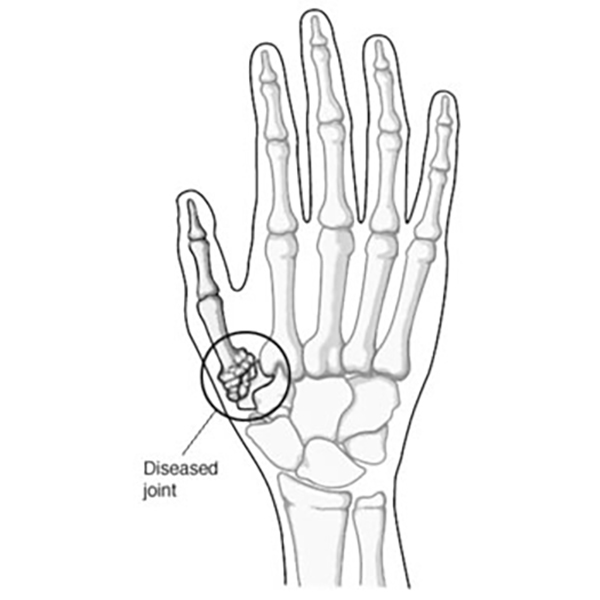
ARTHRITIS OF THE THUMB (CMC ARTHRITIS)
Arthritis is a condition that irritates or destroys a joint. Although there are several types of arthritis, the one that most often affects the joint at the base of the thumb (the basal joint) is osteoarthritis (degenerative or “wear-and-tear” arthritis).
Osteoarthritis occurs when the smooth cartilage that covers the ends of the bones begins to wear away. Cartilage enables the bones to glide easily in the joint; without it, bones rub against each other, causing friction and damage to the bones and the joint.
The joint at the base of the thumb, near the wrist and at the fleshy part of the thumb, enables the thumb to swivel, pivot, and pinch so that you can grip things in your hand. Arthritis of the base of the thumb is more common in women than in men, and usually occurs after age 40. Prior fractures or other injuries to the joint may increase the likelihood of developing this condition.
Symptoms
- Pain with activities that involve gripping or pinching,
such as turning a key, opening a door, or snapping your fingers. - Swelling and tenderness at the base of the thumb.
- An aching discomfort after prolonged use.
- Loss of strength in gripping or pinching activities.
- An enlarged, “out-of-joint” appearance.
- Development of a bony prominence or bump over the joint.
- Limited motion.
Diagnosis
 Your physician will ask you about your symptoms, any prior injury, pain patterns, or activities that aggravate the condition. The physical examination may show tenderness or swelling at the base of the thumb. One of the tests used during the examination involves holding the joint firmly while moving the thumb. If pain or a gritty feeling results, or if a grinding sound (crepitus) can be heard, the bones are rubbing directly against each other. An X-ray may show deterioration of the joint as well as any bone spurs or calcium deposits that have developed.
Your physician will ask you about your symptoms, any prior injury, pain patterns, or activities that aggravate the condition. The physical examination may show tenderness or swelling at the base of the thumb. One of the tests used during the examination involves holding the joint firmly while moving the thumb. If pain or a gritty feeling results, or if a grinding sound (crepitus) can be heard, the bones are rubbing directly against each other. An X-ray may show deterioration of the joint as well as any bone spurs or calcium deposits that have developed.
Many people with arthritis at the base of the thumb also have symptoms of carpal tunnel syndrome, so your physician may check for that as well.
Treatment
In its early stages, arthritis at the base of the thumb will respond to nonsurgical treatment.
- Ice the joint for five to fifteen minutes several times a day.
- Take an anti-inflammatory medication such as aspirin or ibuprofen to help reduce inflammation and swelling
- Wear a supportive splint to limit the movement of the thumb, and allow the joint to rest and heal. The splint may protect both the wrist and the thumb. It may be worn overnight or intermittently during the day.
Because arthritis is a progressive, degenerative disease, the condition may worsen over time. The next phase in treatment involves a steroid solution injection into the joint. This will usually provide relief for several months. However, these injections cannot be repeated indefinitely.
Surgical Options
When conservative treatment is no longer effective, surgery is an option. The operation can be performed on an outpatient basis. Typically the diseased bone is removed, and the joint is reconstructed with a tendon graft.
After surgery, you will have to wear a cast for several weeks. A rehabilitation program, involving a hand therapist, helps you regain movement and strength in the hand. You may feel some discomfort during the initial stages of the rehabilitation program, but this will diminish over time. Full recovery from surgery takes several months. Most patients are able to resume normal activities and are quite satisfied with the results.
